If you’ve ever left a doctor’s appointment feeling like you only got help once something was already wrong, you’re not alone. Traditional medicine excels at treating disease, but it wasn’t designed to prevent it. That’s where Medicine 3.0 comes in.
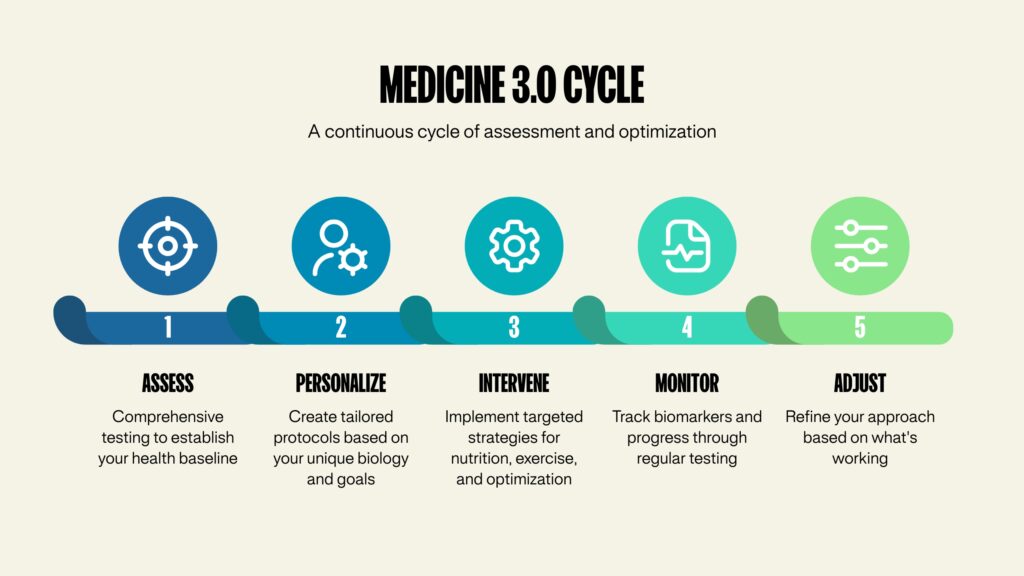
Medicine 3.0 represents a fundamental shift in how we approach health—moving from reactive sick care to proactive health optimization. Instead of waiting for symptoms to appear, this modern framework uses advanced diagnostics, data analysis, and personalized interventions to prevent disease before it starts.
In this guide, we’ll break down exactly what Medicine 3.0 means, how it differs from traditional medical approaches, and why this shift matters for anyone serious about living a longer, healthier life.
The Evolution of Medicine: From 1.0 to 3.0
To understand Medicine 3.0, it helps to see how we got here.
Medicine 1.0: Observation and Tradition (Ancient Times – 1900s)
Medicine 1.0 was based on observation, trial and error, and tradition. Physicians relied on symptoms and bedside manner. Treatment was often more art than science, with limited understanding of disease mechanisms. Without knowledge of germ theory, genetics, or biochemistry, mortality rates from now-preventable diseases remained tragically high.
Medicine 2.0: Evidence-Based Treatment (1900s – Present)
Medicine 2.0 brought the scientific method to healthcare. We developed antibiotics, vaccines, surgical techniques, and evidence-based protocols. This era dramatically improved our ability to treat acute conditions and extend lifespan.
But here’s the problem: Medicine 2.0 is still fundamentally reactive. You develop symptoms, get diagnosed, then receive treatment. It’s excellent for emergencies and acute illness but falls short for chronic disease prevention.
Medicine 3.0: Proactive Optimization (Emerging Now)
Medicine 3.0 shifts the timeline. Instead of treating disease after diagnosis, it focuses on preventing disease from developing in the first place. It combines cutting-edge diagnostics, continuous monitoring, and personalized interventions to optimize health before problems arise. The goal isn’t just extending lifespan (how long you live), but maximizing healthspan (how long you live well).

The Core Principles of Medicine 3.0
Prevention Over Treatment
Medicine 3.0 operates on a simple premise: preventing disease is exponentially easier than treating it.
Take cardiovascular disease. In Medicine 2.0, you might not know you’re at risk until you have chest pain or fail a stress test. By then, arterial damage has been accumulating for years.
In Medicine 3.0, we use advanced lipid panels, coronary calcium scoring, and genetic markers to identify cardiovascular risk decades before symptoms appear. Then we implement targeted interventions—not just to avoid a heart attack, but to prevent arterial disease from starting.
Data-Driven Decision Making
Medicine 3.0 relies on comprehensive data collection and analysis. This means going far beyond the standard annual physical to get a complete picture of your health.
We’re talking about advanced blood work that assesses 100+ biomarkers instead of the typical 10-15. Body composition analysis through DEXA scans reveals your muscle mass, bone density, and visceral fat distribution with precision that a scale or BMI calculation could never provide. Cardiovascular fitness testing like VO2 max gives us objective measures of your aerobic capacity and metabolic health. Some patients even use continuous glucose monitors and wearables to track real-time health metrics. Genetic testing helps us understand your predispositions and personalize interventions accordingly.
This data creates a detailed baseline and allows for tracking changes over time—the only way to know if interventions are actually working.
Personalization
Medicine 3.0 recognizes that what works for one person may not work for another. Generic “healthy lifestyle” advice is replaced with targeted protocols based on your unique biology, genetics, environment, and goals.
Your exercise prescription might prioritize strength training to combat age-related muscle loss, while someone else needs interval training to improve insulin sensitivity. Your dietary approach might require restricting refined carbs due to genetic variants affecting glucose metabolism, while another person thrives on a different macronutrient balance.
Optimizing the “Four Horsemen”
Medicine 3.0 focuses intensive effort on preventing the four major causes of chronic disease and death: cardiovascular disease (heart attacks and strokes), cancer, neurodegenerative disease (like Alzheimer’s and dementia), and metabolic dysfunction (Type 2 diabetes and metabolic syndrome).
Rather than waiting for these conditions to develop, Medicine 3.0 identifies and addresses risk factors 10, 20, or 30 years in advance. This is where the real power of preventative medicine lives—in the decades before disease manifests.

Medicine 2.0 vs Medicine 3.0: A Practical Comparison
Let me paint you a picture. Imagine a 45-year-old executive—successful, busy, seemingly healthy.
The Medicine 2.0 Approach
He goes for his annual physical. The doctor orders a basic blood panel checking cholesterol, blood sugar, and blood pressure. His cholesterol comes back “borderline high” at 210 mg/dL. The doctor says “Let’s watch it” and suggests eating better. There’s no specific plan or follow-up testing scheduled. Five years later, this same patient has a heart attack. How did we miss it?
The Medicine 3.0 Approach
That same 45-year-old comes in for a comprehensive metabolic panel that includes advanced lipids, inflammatory markers, and insulin resistance markers. A DEXA scan reveals visceral fat accumulation that his normal BMI completely missed. VO2 max testing shows declining cardiovascular fitness despite him “feeling fine.” A coronary calcium score detects early arterial calcification. His ApoB level reveals high cardiovascular risk despite that “normal” total cholesterol number.
Now we have a complete picture. We develop a personalized intervention plan with specific dietary changes, a structured exercise program, and possibly medication. We monitor quarterly to track improvement. The result? Heart disease prevented, not just treated after the damage is done.
The Key Difference
Medicine 2.0 asks: “Are you sick yet?”
Medicine 3.0 asks: “How can we keep you from getting sick?”
What Medicine 3.0 Looks Like in Practice
Comprehensive Baseline Assessment
A Medicine 3.0 approach starts with understanding exactly where your health stands today. This goes far beyond a standard physical.
We’re looking at advanced blood testing covering 100+ biomarkers versus the standard 10-15. Body composition analysis assesses muscle mass, fat distribution, and bone health with precision. Cardiovascular fitness testing measures your aerobic capacity. We evaluate metabolic health including glucose tolerance and insulin sensitivity. And we take a detailed health history covering lifestyle factors, family history, and environmental exposures that might affect your risk profile.
This isn’t just collecting data for the sake of it. Every test serves a specific purpose in understanding your current trajectory and identifying opportunities for intervention.
Ongoing Monitoring and Adjustment
Health isn’t static, so neither is Medicine 3.0. Regular testing tracks how your body responds to interventions and how your health trajectory changes over time. This allows for course correction before small issues become big problems.
Think of it like piloting a plane. You don’t just set the controls at takeoff and hope for the best. You constantly monitor instruments and make tiny adjustments to stay on course. Your health deserves the same level of attention.
Evidence-Based Interventions
Medicine 3.0 interventions focus on what actually moves the needle, not what sounds good in theory.
Exercise becomes medicine with specific protocols for strength, cardiovascular health, and metabolic function. Nutrition gets tailored to your metabolic health and goals rather than following whatever diet trend is popular this month. Sleep optimization becomes a priority because poor sleep accelerates all chronic disease processes. Stress management reduces inflammation and improves resilience. Strategic supplementation happens based on testing, not guesswork. And when appropriate, medications help optimize metabolic health and reduce disease risk.
Every intervention is chosen deliberately based on your data and adjusted based on results.
Who Benefits Most from Medicine 3.0?
While everyone can benefit from proactive healthcare, Medicine 3.0 is particularly valuable for certain groups.
High Performers and Executives
If your career demands peak cognitive and physical performance, you can’t afford to wait until something breaks. You need to maintain high performance while building resilience for the long term. Medicine 3.0 helps you optimize both immediate function and long-term health simultaneously.
People with Family History of Chronic Disease
If heart disease, diabetes, cancer, or Alzheimer’s runs in your family, you’re starting with higher risk. But here’s the thing: genetic predisposition isn’t destiny. Medicine 3.0 gives you the tools to potentially overcome genetic risk through early intervention. We catch problems in the dysfunction phase, before they become disease.
Anyone Over 40
The risk of chronic disease accelerates after 40. This is when Medicine 3.0 makes the biggest difference—catching and reversing early dysfunction before it becomes irreversible disease. The interventions we implement in your 40s and 50s determine your health trajectory for the next several decades.
People Who Want to Maximize Healthspan
If your goal isn’t just living longer, but living well—staying active, independent, and mentally sharp into your 70s, 80s, and beyond—Medicine 3.0 provides the roadmap. It’s not about adding years to your life at any cost. It’s about adding life to your years.
The Limitations of Medicine 2.0 (That Medicine 3.0 Addresses)
Problem 1: “Normal” Doesn’t Mean Optimal
Standard lab ranges are based on population averages, which include a lot of unhealthy people. Your cholesterol might be “normal” while still significantly increasing your risk for heart disease. Your fasting glucose might be “fine” while your insulin levels reveal metabolic dysfunction that won’t show up as diabetes for another five years.
Medicine 3.0 uses optimal ranges based on longevity research, not just population norms. We’re not asking “Are you as healthy as the average American?” We’re asking “Are you as healthy as you could be?”
Problem 2: Annual Checkups Aren’t Enough
Once a year is too infrequent to catch problems early or assess if interventions are working. Think about it: if you only checked your bank account once a year, you’d have no idea if you were on budget until it was too late to course correct.
Medicine 3.0 involves more frequent monitoring during active optimization phases, then regular maintenance testing to ensure you stay on track. This creates accountability and allows for rapid adjustment when needed.
Problem 3: Symptom-Based Care Misses Early Disease
By the time you have symptoms, disease has often been progressing for years. Type 2 diabetes has typically been developing for 7-10 years before diagnosis. Alzheimer’s-related brain changes start 20+ years before memory loss appears. Cardiovascular disease silently progresses until that first heart attack.
Medicine 3.0 uses biomarkers and advanced testing to detect dysfunction years before symptoms appear. We intervene when problems are small and reversible, not after they’ve become chronic conditions requiring lifelong management.
Problem 4: Generic Advice Doesn’t Account for Individual Variation
“Eat less, move more” fails because it ignores metabolic differences, genetic factors, and individual circumstances. Some people are insulin resistant and need to drastically reduce carbohydrates. Others do fine with higher carb intake but struggle with dietary fat. Some people respond beautifully to moderate exercise while others need high-intensity intervals to see metabolic improvements.
Medicine 3.0 personalizes every recommendation based on your unique biology and context. What works for your neighbor might not work for you, and that’s okay. We find what works for your body.
The Science Supporting Medicine 3.0
The Medicine 3.0 framework isn’t speculation—it’s built on decades of longevity research.
Studies consistently show that cardiovascular fitness (measured by VO2 max) is one of the strongest predictors of longevity, more powerful than many traditional risk factors we’ve focused on for years. Research demonstrates that visceral fat (measured via DEXA or similar imaging) predicts metabolic disease risk better than BMI or weight alone. Data proves that early intervention on metabolic markers like insulin resistance, inflammation, and lipid particles can prevent or reverse disease progression. Longevity studies across multiple populations consistently show that preventing chronic disease is more effective than treating it after diagnosis.
The tools of Medicine 3.0—advanced testing, personalized protocols, continuous monitoring—allow us to apply this research at the individual level rather than just at the population level.
Getting Started with Medicine 3.0
Transitioning to a Medicine 3.0 approach doesn’t require abandoning your current healthcare. Instead, it means augmenting it with proactive, preventative care.
The first step is getting a comprehensive assessment that goes beyond standard panels. This should include advanced metabolic markers, body composition analysis, and fitness testing that paint a complete picture of your current health status.
Next, you use those test results combined with your health history to identify your specific risk factors. Are you at risk for cardiovascular disease based on your lipid profile and family history? Is metabolic dysfunction brewing based on your insulin levels and visceral fat? Are you losing muscle mass faster than you should be?
Once you understand your risks and goals, you develop a personalized protocol. This isn’t generic advice—it’s a specific plan for exercise, nutrition, sleep, stress management, and any necessary medications or supplements tailored to your situation.
Finally, you monitor and adjust. You retest regularly to see what’s working and what needs adjustment. Your protocol should evolve as your health improves and your life circumstances change. What you need at 45 might be different from what you need at 55 or 65.
Common Questions About Medicine 3.0
Is Medicine 3.0 only for wealthy people?
Let’s be honest: comprehensive preventative care does require investment. But here’s what people miss—the cost of chronic disease, both financial and personal, is far higher. A heart attack, diabetes management, cancer treatment, or dementia care will cost exponentially more than preventative intervention, not to mention the toll on quality of life.
Additionally, many Medicine 3.0 principles like prioritizing exercise, sleep, and stress management cost nothing. The testing and medical oversight require investment, but the lifestyle interventions are accessible to anyone willing to prioritize them.
Will my insurance cover Medicine 3.0 approaches?
Insurance is designed around Medicine 2.0, which means it covers treating diagnosed conditions. Most advanced testing and preventative protocols aren’t covered because they’re not treating an active disease. This is frustrating but understandable given how insurance is structured.
This is why many people invest directly in their health through concierge medicine models or direct-pay preventative care. They view it as an investment in avoiding future medical costs and maintaining quality of life rather than as an expense.
Can I practice Medicine 3.0 with my current doctor?
Some physicians are adopting Medicine 3.0 principles, but most traditional practices don’t have the time or infrastructure for this level of personalization and monitoring. The standard 15-minute appointment slot doesn’t allow for the kind of deep engagement Medicine 3.0 requires.
Many people work with a preventative medicine specialist or concierge physician alongside their primary care physician. Your PCP handles acute issues and routine care, while your Medicine 3.0 provider focuses on optimization and prevention.
Isn’t this just “wellness” or “functional medicine”?
Medicine 3.0 shares goals with these movements but is more rigorous. It’s deeply rooted in evidence-based medicine, uses advanced diagnostics, and focuses specifically on preventing the major causes of death and disability—not just optimizing how you feel day-to-day.
Feeling good is great, but Medicine 3.0 is concerned with objective health markers that predict long-term outcomes. You can feel fine while arterial disease silently progresses. Medicine 3.0 catches those problems regardless of how you feel.
The Future is Proactive
Medicine 3.0 represents a fundamental rethinking of healthcare—from reactive treatment to proactive optimization. It acknowledges that waiting for disease to develop, then trying to treat it, is neither the most effective nor the most humane approach.
For people who want to live not just longer, but better—maintaining physical capability, mental sharpness, and independence well into later decades—Medicine 3.0 provides the framework and tools to make that possible.
The question isn’t whether Medicine 3.0 will become the standard of care. The question is: How long will you wait to adopt it for yourself?
The reality is that chronic disease doesn’t develop overnight. It’s the result of decades of small dysfunctions compounding into diagnosable conditions. But that also means we have a massive window of opportunity to intervene. The choices you make today about testing, monitoring, and optimization will determine your health trajectory for the next 20, 30, or 40 years.
Every year you wait is a year of potential dysfunction you’re not catching or reversing. And while it’s never too late to start, the earlier you begin, the more dramatic the impact.
Ready to Experience Medicine 3.0?
At Preamble Health, we’ve built our entire practice around Medicine 3.0 principles. From advanced diagnostics like DEXA scans and VO2 max testing to comprehensive blood work and personalized health optimization plans, we focus on preventing disease and maximizing healthspan.
We work with anyone who refuses to wait for disease to develop before taking action. If you’re ready to take control of your health trajectory, we’re here to guide you.
Learn more about our approach:
- Medicine 3.0 Executive Physical – Our comprehensive health assessment and optimization program
- Advanced Blood Work Analysis – Go beyond basic panels to understand your metabolic health
- DEXA Scans – Precise body composition and bone density analysis
- Schedule a Consultation – Discuss your health goals with our team